Getting older can be a real pain in the neck… and the back, too.
For many people, that pain can be caused when their bones and discs begin to deteriorate. We call this degenerative disc disease. It’s also sometimes referred to as spondylosis.
Not everyone with degenerative disc disease will have severe pain, but you should know that it’s a common cause of both lumbar pain (low back pain) and cervical pain (neck pain), especially as you age. In fact, statistics show that 40% of people over the age of 40 suffer from some form of degenerative disc disease.
And that number increases to more than 80% for people over 80.[i]
It’s important to keep in mind that it’s possible to have pain from herniated discs or pinched nerves and not have excessive disc degeneration.
In this article, we’ll cover the risk factors, causes, symptoms and of degenerative disc disease. At the end of this article, you will find recommended treatment options and provide a video showing spinal decompression stretches for back pain.
What Is Degenerative Disc Disease?
Degenerative disc disease (DDD) isn’t really a “disease” at all. But it’s the term we use to refer to the typical changes that take place in your spinal discs over your lifetime. Although degenerative disc disease can occur in any part of the spine, it most often occurs in the lumbar spine (your lower back) or the cervical spine (your neck).
It helps to understand what your spinal discs are and what they do…
Spinal discs are soft, compressible discs that separate the vertebrae. They serve as shock absorbers between the bones of the spine. These discs are designed to help your back stay flexible and sturdy.
They prevent injury or trauma that can occur when you perform daily activities… everyday movements like twisting, flexing and bending.
Think about how often you do these things… lifting your grandkids, swinging a golf club or tennis racket… even bending down to pick up something you dropped on the floor…
As you can imagine, your spinal discs experience a lot of wear and tear over the years.
The discs start to break down. This breakdown can sometimes lead to degenerative disc disease.
Common Risk Factors for Degenerative Disc Disease
Unfortunately, it’s normal for disc degeneration to occur as we age. But there are some things that can accelerate the process, like:
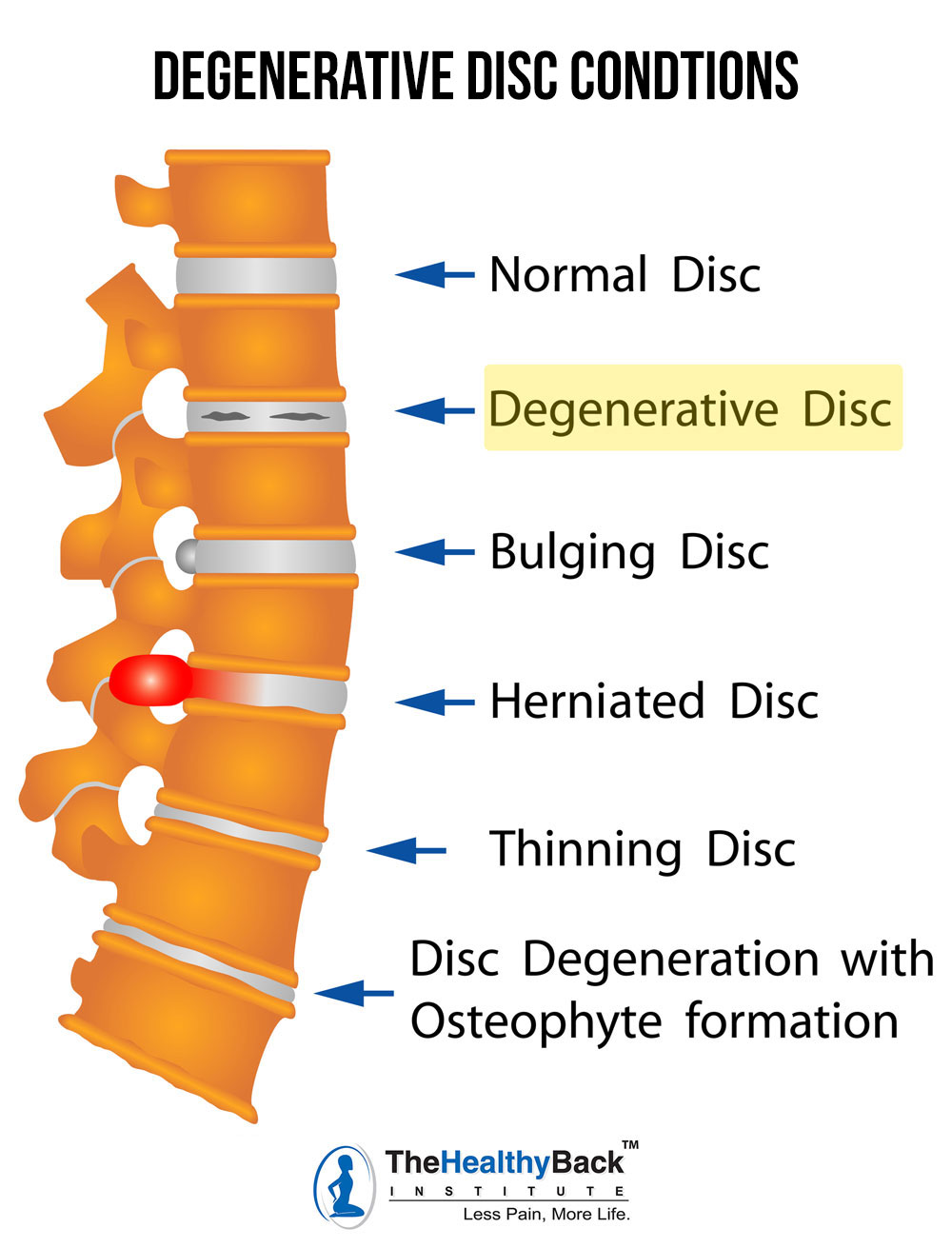
- Tiny cracks and tears in the annulus (outer layer) of the disc. If this happens, the (disc) may be forced out through these tears. This can cause to rupture, bulge or break into fragments.
- Loss of fluid in discs that reduces their ability to act as shock absorbers and causes them to be less flexible.
Sudden injuries, such as car accidents, falls and sports injuries, and poor nutrition can also begin the degeneration process.
When there is less padding between the spaces in the vertebrae the spine becomes less stable. Osteophytes (bone spurs) can form as your body attempts to distribute weight more evenly after a disc has been damaged. These tiny bone outgrowths can end up irritating and damaging the nerves in your spinal column. This can be extremely painful!
Common Symptoms of Degenerative Disc Disease
Your pain levels are not a good indicator of how much disc damage you actually have. (And again, you could have damage and have no pain at all.)
But if you are experiencing pain, you’ll find that the pain is worst in the location of the affected disc.
If you’ve experienced lumbar disc damage or lower back pain for many years, you will experience radiating pain down your buttocks, thigh and knee. You may also have symptoms that include numbness or tingling in the legs and lower back. Sciatica is also a common symptom for those who suffer ongoing lower back pain.
If your symptoms include neck pain that radiates throughout the shoulders and arms, you may have cervical disc damage. These symptoms also include tingling and numbness in the neck and shoulder region as well as a decreased range of motion. This pain may worsen with long periods of sitting or poor posture.
Common Causes of Degenerative Disc Disease
Yes, aging is one cause of degenerative disc disease, but it’s not the only one. Regular wear and tear and excess movements can also contribute to DDD.
There are many lifestyle factors that can lead to conditions that cause degenerative disc disease. Even what you do for a living can play a major role. For example, people who work in physical industries like construction or sanitation are more likely to suffer from osteoarthritis or a herniated disc – both conditions that can lead to a deterioration of spinal discs.
Obese people and those who smoke cigarettes are also more likely to have symptoms of degenerative disc disease. It’s believed this is because they are more likely to lead a sedentary lifestyle.
Muscle imbalances – essentially, one set of muscles overpowering another – create “postural dysfunctions” that put abnormal pressure on a disc and cause increased wear and tear over time. Eventually, the weak spot gives way and makes contact with the nerve, bringing pain.
Here are some other conditions that can lead to disc deterioration:
- Spondylolisthesis: a spinal condition in which one vertebrae slips backward or forward relative to the next vertebrae. This condition can cause a compression of nerve roots and cartilage deterioration. In addition to causing pain to your sciatic nerve, this can lead to further deterioration of the spinal discs. Many of the symptoms of degenerative disc disease mirror those of sciatica. That’s partially because sciatica is one of the main symptoms of degenerative disease. Of course, this doesn’t mean that every person who suffers from sciatica will end up with DDD. Because of this though, there are several medical problems related to sciatica that can cause degenerative disc disease.
- Lordosis: a condition that occurs when the lumbar or cervical vertebrae (lower back or neck) column is partially curved. This can manifest as a weak leg or thigh, an area often affected by sciatica. This curvature can lead to spinal degradation over time, which may eventually lead to degenerative disc disease.
- Herniated disc: An abnormal bulge or bursting of a spinal disc. Even once a herniated disc has been fixed with surgery, the destruction to the disc will continue over time. Each movement you make over the years is slowly causing your disc to slowly deteriorate.
- Osteoarthritis: Also known as degenerative arthritis, this occurs when the cartilage between your joints breaks down. The cartilage can wear out because of daily wear and tear, aging, injury or misuse. When this occurs in the spine, your discs are not being protected or cushioned from general movement. This means that every step you take, every twist and bend is putting stress on your discs.
- Spinal stenosis: A condition in which the spinal canal narrows, compressing or “squeezing” the spinal cord and nerves inside. The narrowing also causes increased friction between your discs as you move. As the space decreases around the spinal cord, bone spurs will develop. These bone spurs (as I mentioned above) put additional pressure on the spinal cord and nerve roots.
Degenerative Disc Disease Treatment Options
Most doctors have a standard course of treatment for degenerative disc disease.
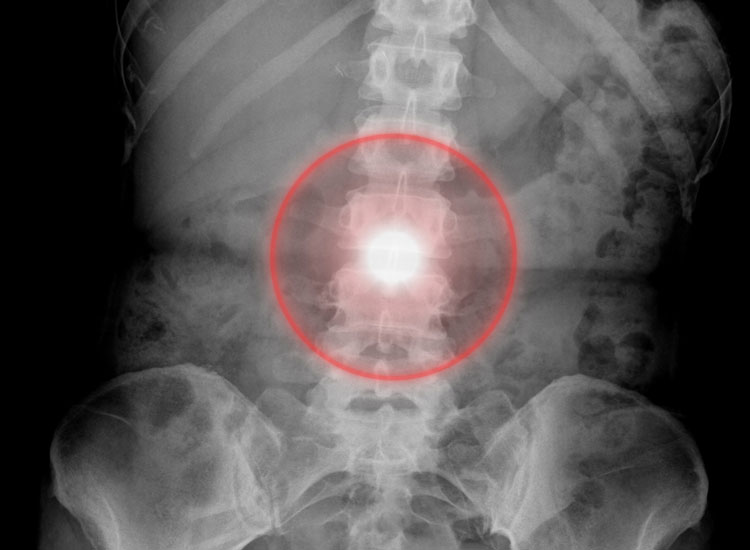
They’ll perform a physical examination and reviewing your medical history to see if any of your daily activities could be causing your pain. They may check for muscle weakness and numbness, Then they’ll likely order an x-ray, MRI (magnetic resonance imaging) or CT scan they’ll likely suggest one or more of the following treatment options:
-
- Non-steroidal anti-inflammatory drugs (NSAIDs such as ibuprofen) and other pain medications
- Ultrasound
- Electrical stimulation
- Therapeutic exercises and physical therapy
Spine surgery is also an option, with the two main goals being to take pressure off the nerve and stabilize the joints.
Some of these treatments, such as ultrasound and hot packs, are conservative treatments. Others — like cortisone injections and pain medications like ibuprofen — are harmful to your health. They can have terrible – and potentially fatal – side effects. But most of them also FAIL — because they simply address your symptoms.
They don’t address the cause of your degenerative disc disease.
Conventional doctors focus on pain management,
Think about it…
They don’t really want to cure you. Once your pain is “fixed,” you don’t need them anymore. And they stop profiting from your pain.
I want you to understand mainstream medicine’s treatment options aren’t your only options.
Your degenerated disc is a physical problem, and it requires a physical solution. There are no pills or injections that can create postural balance in your body, which is what is necessary to reduce the pressure on the nerve.
Unfortunately, some cases of degenerative disc disease DO require surgery, but that should only be a last resort. There are plenty of nonsurgical treatment options you can use for pain relief. And you can use them right in your own home.
Our Suggested Treatment Options
- Try Muscle Balance Therapy™. The principles of treatment address both the pain of a degenerative disc and the root of the problem – in other words, what’s causing the pressure in the first place. Through strategic body assessments, your individual muscle imbalances can be identified. Once that is done, a very targeted corrective program can be designed for your specific needs. [Learn more]
- Use Hot and Cold Therapy. Apply a cold compress to the affected area for 20 minutes. After that, switch to a hot compress for 20 minutes. The Healthy Back Institute offers a state-of-the-art heating pad with infrared heat that’s been shown to melt away pain and restore mobility in just 10 minutes.
- Skip the OTC Painkillers. Instead of popping an Advil or Tylenol to relieve your pain, opt for a natural pain reliever that won’t put your health at risk. If you’re looking for immediate short-term pain relief you may want to consider a topical pain cream like our Rub on Relief® and a natural pain relief supplement with proteolytic enzymes, which can be found in our product, Heal-n-Soothe®.

You have the best explanation of my back ever. So when someone asks me all I have to do is bring up this page and have them read it.
I rode dirt bikes, played sports. Then worked assembly 15 yrs (hands are shot) in those years played baseball for the bars and rode Harleys. Found myself in bed for year and half had to learn to walk all over again cause husband didn’t have ins. different story. He’s not around anymore. I’m in AZ.now took care of Mom. She passed and my life is mine again. I want to dance walk hike and do things. Tired of shots phy. Therapy and taking all those meds.
Hi my name is Debbie and Have osteoarthritis I was diagnosed with with dad as you call it. It is very painful, every day and night it never goes away and I refuse all those pills the Dr wants me to take, I did at first try them all but got off of them right away after hearing the side affects. I took Gabapenten, steroids, Ibuprophren, and a couple of others. Nothing worked. So now I don’t know what to do I can barely walk at times and my active life is no more, I don’t go to far from in case I need to lay down and that’s quite often. I have had exrays, MRI’s catscans etc. Even physical therapy, the only thing I liked was being in the pool, it helps some while your in it. I did alot of physical work over the years and Alot of dancing which I love and now I can’t even do that. I feel as if I have no life I’m very limited. Thank you for the information. I’ve got to try this treatment. I’ve also learned to eat healthier and I’m into alot of things that are natural to help with swelling like ginger mixed with other fruits and vegetables and it really works great at keeping the swelling off which causes pressure. I was thinking of trying the Keto diet. So I will be ordering this and I really hope this works I’m so exhausted from all of this Chronic pain. Thank you for your explanations and information because that is me and I need some help.
HI Debbie,
Thank you for your comment and explanation regarding your osteoarthritis. We would like to help and a good starting point is our Book the 7 Day Back Pain Cure.
The book discusses back pain and related issues along with treatment options and pain relief suggestions. Please read more information about it via the link below
https://losethebackpain.com/products/7-day-back-pain-cure-book
We have also sent you an e mail regarding Arthritis, please look out for it.
Thank you. Our Best Wishes
Admin (The Healthy Back Institute)
Hello,it sounds like your on the right track. If you look at the ingredients in these supplements their amazing and just what we need, it’s not always convenient to get enough of these so this supplement is crucial but I would also buy the natural food sources for them,cook with them add them to smoothies, anyway you can get more of them you’ll greatly benefit from it. Stay away from the breads,pastas ect… and get enough clear fluids. Also it seems even one night with little or no sleep can trigger flair ups so proper rest is important. Your right about the drugs that conventional Dr’s give being bad,gabapentin and steroids are terrible. Cause edema,swelling and have many more bad side affects. I would also start detoxing with celery juicing and I recommend following Anthony the medical medium. He’s amazing,has all the answers and if you follow him on social media you’ll get constant updates on many amazing natural food sources to help you on your healing journey. Good luck and God bless
Yes I want the newsletter cause you gave the best explanation of eveything I have that tells me you know what your talking about.
Of course I have more but don’t want to overwhelme you. Ha ha like I could do that.
I finally received my heal and soolth yesterday, last night took 3. This morning 2, still took my meds. I’m going to see how it’s going to go. I have my fingers crossed. I know I can go up but I did like to take a lot of pills. My first disc went when I was 18 yrs old I’ve been on disablity since 98 I’m 58, you tell me.
Theirs are ways to reverse these symptoms and prevent it from progressing. We just weren’t tought anything different. Conventional Dr’s are clueless on natural cures and don’t give their patients those tools. All the ingredients in these supplements are amazing and will help you. My advice would be to continue these but also use the natural food sources for these to cook with in smoothies, anyway you can. Their are many benefits in detoxing as well,celery juicing. I recommend Anthony the medical medium. If you follow him on social media you’ll get constant reminders on so many healing foods and their benefits plus a wealth of information and knowledge that will help you on your healing path. Getting enough clear fluids and staying away from pastas, breads and all those foods that are terrible for arthritis is key as well. Ok,good luck and god bless
I understand what you are saying. I had a two level fusion in October, 2009. I’ve been on disability since. I am in pain constantly. I want my life back. I try to stay positive, but when pain controls your thinking, it gets tough.
Hi my name is Tina Norgaard.Live in Canada.Just orderd the product .At 35 i was already diagnosed with evey bone trouble.DDD and sacroiliac desease stenosis of the spine osteoarthritis .One year ago had a bike accident broke my neck 5 months.in rehab.Ang got a Bakercyst in my left knee now all swolen up needs to be drained.Right hip very bad bursitis.walk with 2 canes of and on.So im looking forward to use this product and get a bit of an improvement.
Hi Tina,
Thank you. You may also like to consider getting yourself a copy of and reading our book the “7 Day Back Pain Cure”.
We feel education is key to understanding and addressing back pain issues. The book discusses back pain and related conditions, pain relief methods to try, treatment options, causes of back pain, pain relief action plans and other helpful information related to back pain, which you may find useful to consider.
Please read more details about the 7 Day Back Pain Cure book via the link below
https://losethebackpain.com/products/7-day-back-pain-cure-book
We wish you well, Thank you
Admin (The Healthy Back Institute)
Thanks, for this information. I do have a Bulging Disk since 2009. Have received shots every 4 months since then and now they are not working. So, I take prescription for it. My Dr. told me, there is nothing more he can do for me. I am 83 yrs old and still can move fast.
HI Olivia,
Thank you. We would like to suggest you consider getting yourself a copy of and reading our book the “7 Day Back Pain Cure”.
The book discusses back pain and related conditions, pain relief methods to try, treatment options, pain relief action plans and other helpful information related to back pain, which you may find useful to consider.
Please read more details about the 7 Day Back Pain Cure book via the link below
https://losethebackpain.com/products/7-day-back-pain-cure-book
Our Best Wishes
Admin (The Healthy Back Institute)
in 2009, I was 45, lean little machine and had a big problem of comparing myself to men that could be my son as far as physical fitness. Well, decided to to some “light weight” clean and jerks past what my core could handle. Felt great, went home and wok up the next morning in the worst pain I have ever been in my life. Sciatica on right lower back down my butt, on outer leg and into my 2 little right toes. At one point, it felt like someone was taking a knife and cutting the skin between my toes. The only way to take the pain away was to lay down flat (decompress) or sit on a basketball or smaller 8″-10″ ball that allowed me to extend my lower back. Also, sitting on the toilet helped (I guess because the back sort of sinks down in a hole. FFW to today, been addicted to many pain meds and kicked all of them; oxycontin, hydrocodone, oxycodone, fentanyl, and finally weaned my way down to Beupenorphine 8mg oral sublingual 1x day in the morning and looking to get off that. All the MRIs and discograms done early on or when I re-inured as a result of torquing motion showed torn disc S1/L5 level 5 tear, L4/L5, level 4 tear. Tears have long since healed but still feel like I have a knife stabbing in my low back S1/L5, L4/L5. I’ve gotten more used to it and just live with it but I have 2 little boys; 2 and 5 that I have to keep up with as I will be 55 in June. I tried my 1st bottle of Heal and Soothe and felt like I was getting results until I was trying to unload a 450lb motorcycle from my truck by myself and flipped out of the bed with the bike landing on top of my legs. I also feel like the product causes a bit of upset lower stomach causing a diarrhea. I want to stay on Soothe and Heal but haven’t been taking as Jesse suggested. Keep going and the lower stomach stuff will resolve? I have always been the kid that threw up after drinking orange juice on an empty stomach.
Hi Richard,
Thank you for sharing your experiences. We believe education is key to addressing back pain issues and would suggest you please get yourself a copy of our book the “7 Day Back Pain Cure”.
The book discusses back pain, sciatica and related conditions, pain relief methods to try, treatment options, pain relief action plans and other helpful information related to back pain and sciatica.
Please read more details about the 7 Day Back Pain Cure book via the link below
https://losethebackpain.com/products/7-day-back-pain-cure-book
Our Best Wishes
Admin (The Healthy Back Institute)
Hello
At the age of 24, I had surgery for a herniated disc in L5S1 because of a paralysing hernia. As a result, I was relueved for about 6 months, then pain returned very regularly. I suffered almost all my professional life (I was a nurse).
To alleviate, I had a very heavy TT (including morphine patches when pain too disabling), because I always wanted to continue working. I had many infiltrations over the years, and I went regularly to a pain center twice a week, where I was doing relaxation among others.
In 2009, I found myself hospitalized because I remained blockef (thus operated on’the left meniscus); a month later, the gall bladder, and 3 months later, I was made a first lumbar arthrodesis, L4/l5/L5/S1; it took a few monts later because transplant did not take.
In short, today I am 66, and although the pain is much less intense, it is none the less true that I do suffer from chronic pain that never leave me ( it means day & night)!
With self-hypnosis, I ´m not doing too badly, but in fact my wish is to stop completely the only medecine I continue to take (Contramal 150 mg et 100 mg). And the only way I could do this would be by usingr of TEN’S, this device which sends diverse programs of electric currents via electrodes, because this calmed me a lot. Unfortunately, here in France, only pain clinics are authorized to prescribe it, but I do not go there anymore.
Would you have this chap of divice? If you do, would it be possible for me to acquire it and at which price?
Sorry for the length of this e-mail, but it’s not so easy to synthesizevmore tan 40 years of pain!
Very cordially.
Thémy
BONNAIRE, sorry we do not sell TENS devices but you can get them on Amazon, here in the States…
Thanks
Steve
I have cervical neck fusions.
The symptoms that led me to surgery was mostly numbness in the fingers caused from the neck.
This was a great reading. It really caught my interest since I know many people with back problems. Although the advice in this article is great I think there is an underlying problem. I have seen that if the hip flexors are tight people have a greater risk of having back pain in their later years.
Hi Fredrik,
You’re absolutely right – tight hip flexors, often from extended sitting, are a common issue along with many other muscle imbalances. While we didn’t address those in detail in this article, we do in the article on Muscle Balance Therapy we linked to. You also may find this article on The 17 Muscles Causing the MOST Back Pain (including hip flexors) to be helpful.
Best wishes,
Steve
Thanks Jesse this is the first time in years any one has every tell me what was wrong with my back so I am very greatful for the info and I will be doing this every
Day .
What do these initials stand for:
Jesse Cannone, CFT, CPRS, MFT
Hi Damian,
Thank you for your question. Please see the following link for more information.
https://losethebackpain.com/medical-advisory-board/jesse-cannone/
Thank you
Admin
(The Healthy Back Institute)
This article implies that doctors have no interest in a cure and that doctors are only interested in symptom management When all along we know there is no cure and that symptom management is the only option. Doctors know this, they admit this to themselves and their patients. Don’t be so arrogant as to imply that there is a cure they are holding back from the public.
This sounds great!
Good Day to you all,
My question is rhetorical I think. Do chemicals such as Carbon Tetrachloride, Agent Orange, and Chemo have anything to do with Disc Degeneration?
I spent 17 months in Vietnam where I was exposed to Agent Orange at least 4 or 5 times a week, Carbon Tetrachloride 7 days a week, and Diesel fuel also daily.
State Side I was exposed to Carbon Tetrachloride 7 days a week, and Diesel fuel also daily.
While stateside and stationed at Camp Lejeune I was exposed to the Chemically charged Camp underground water system.
Do you feel that all of these exposures could be causing my degeneration disc and Neuropathy? if so can you point me in the correct direction for some research materials I can use against the VA.
While I can not comment on those specific agents I will say that in general, when the body has an immune response to anything and inflammation is running high the body will breakdown over time, there is just now way around that. So doing everything you can to support your body can help the sooner you do it the better and being consistent with those supportive measures is the trick to success.
https://emedicine.medscape.com/article/1175276-overview
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4492068/
https://www.ncbi.nlm.nih.gov/pubmed/8972163
https://www.foundationforpn.org/what-is-peripheral-neuropathy/causes/toxins/
This article explained a lot what’s going on with my back. Especially the off balance part. In 1951 I had polio, consequently my right leg is weaker than my left. Now in my 70’s, I fall easily since I don’t have good balance. I have been in 3 bad auto accidents (never the driver) and in 1997, I had 2 back surgeries. For going on 20 years, I was relatively pain free. But now the pain is constant and sometimes 10+. I have had 4 injections in my back and 6 in my neck. Neck is fine but the back, not so much. Next step is surgery. NOT!
Can the proteolytic enzymes contained in Heal and Soothe cleave collagen polypeptides?
Bob, That is a possibility, that is why we ask you to take the enzymes on an empty stomach.
I really wanted to try this product but I saw I video on who shouldn’t take it and one of them was if you’re on a blood thinner. I am on a blood thinner Elquis have had 3 blood clots so I decided not to take It.
Ann, Thank you, we take the safety of our customer a primary and have for the past 17yrs. Thanks
I have severe scoliosis from cervical to lumbar, I will be getting injection in my neck but I gave 2 Tarlov cysts in sacrum, do you know anything about them??
Hello Ourania,
We would suggest that if you have questions and are seeking medical advise to ask your primary care physician. They will be more familiar with your medical history to help you best.
Thanks,
James HBI-Staff